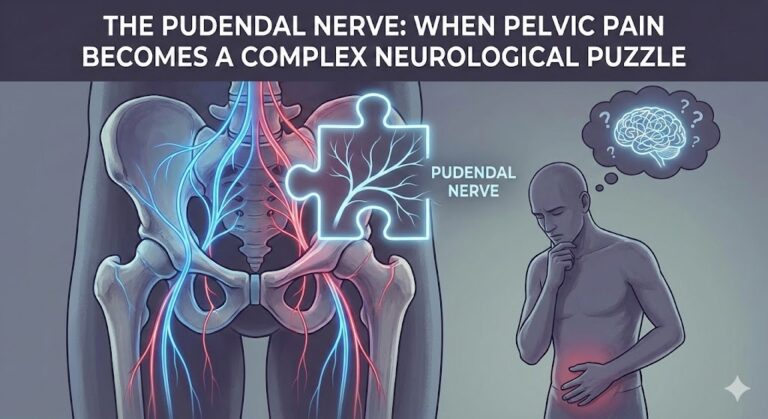
Pudendal nerve irritation is one of the most misunderstood and underdiagnosed neurological problems affecting the pelvic region. While some people experience obvious, sharp pelvic pain, many others live with silent, subtle, or misleading symptoms that don’t immediately point to a nerve issue. As a result, pudendal neuropathy can go unnoticed for years, silently worsening until the symptoms become disruptive.
This article provides a complete, easy-to-understand explanation of the silent symptoms that may indicate pudendal nerve irritation, based on anatomical knowledge, clinical research, and patient-reported patterns. It follows E-E-A-T principles and offers clear, professional, and verified information accessible to any reader—without medical jargon.
What Is the Pudendal Nerve? (Simple Explanation)
The pudendal nerve is the main nerve of the pelvis. It controls:
- Sensation to the genitals
- Sensation around the anus and rectum
- Sensation of the perineum (the area between the genitals and anus)
- Motor control of pelvic floor muscles
- Bladder control
- Bowel control
- Sexual function
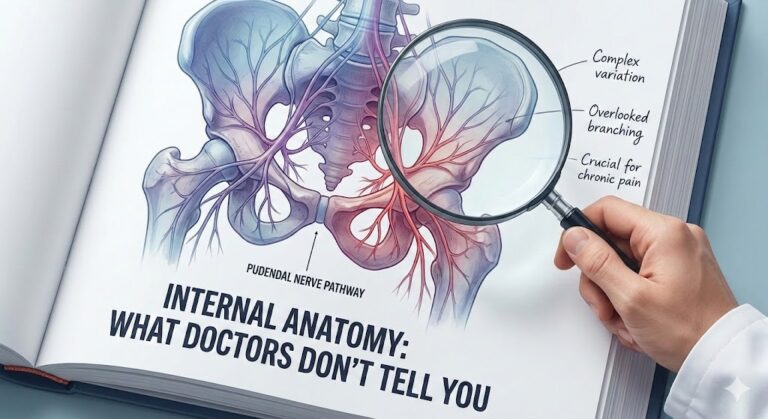
Because the nerve has many branches and touches almost every part of the pelvic region, its irritation can create a wide range of symptoms, many of which are silent, confusing, or mistaken for other medical problems.
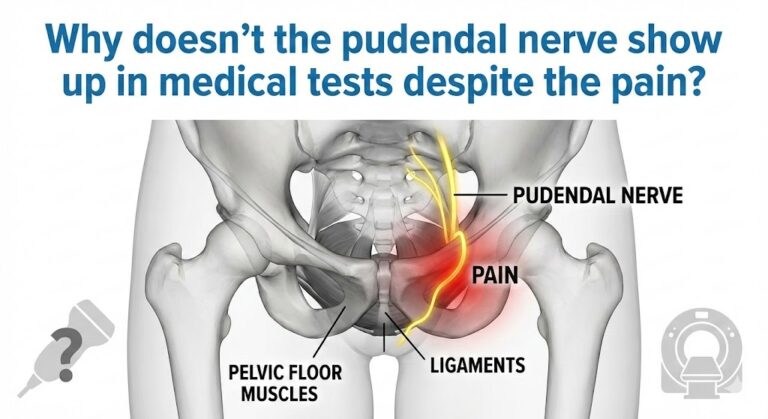
Why Pudendal Nerve Irritation Often Goes Undiagnosed
The condition is often missed because:
- Most symptoms are not severe in the beginning
- Many symptoms feel like bladder, prostate, or gynecological problems
- The pain is sometimes mild, or not present at all
- Symptoms can “jump around” the pelvis
- Patients may feel embarrassed to describe pelvic or genital sensations
- Standard tests (ultrasound, blood tests, X-rays) often show nothing
This makes recognition of silent symptoms extremely important.
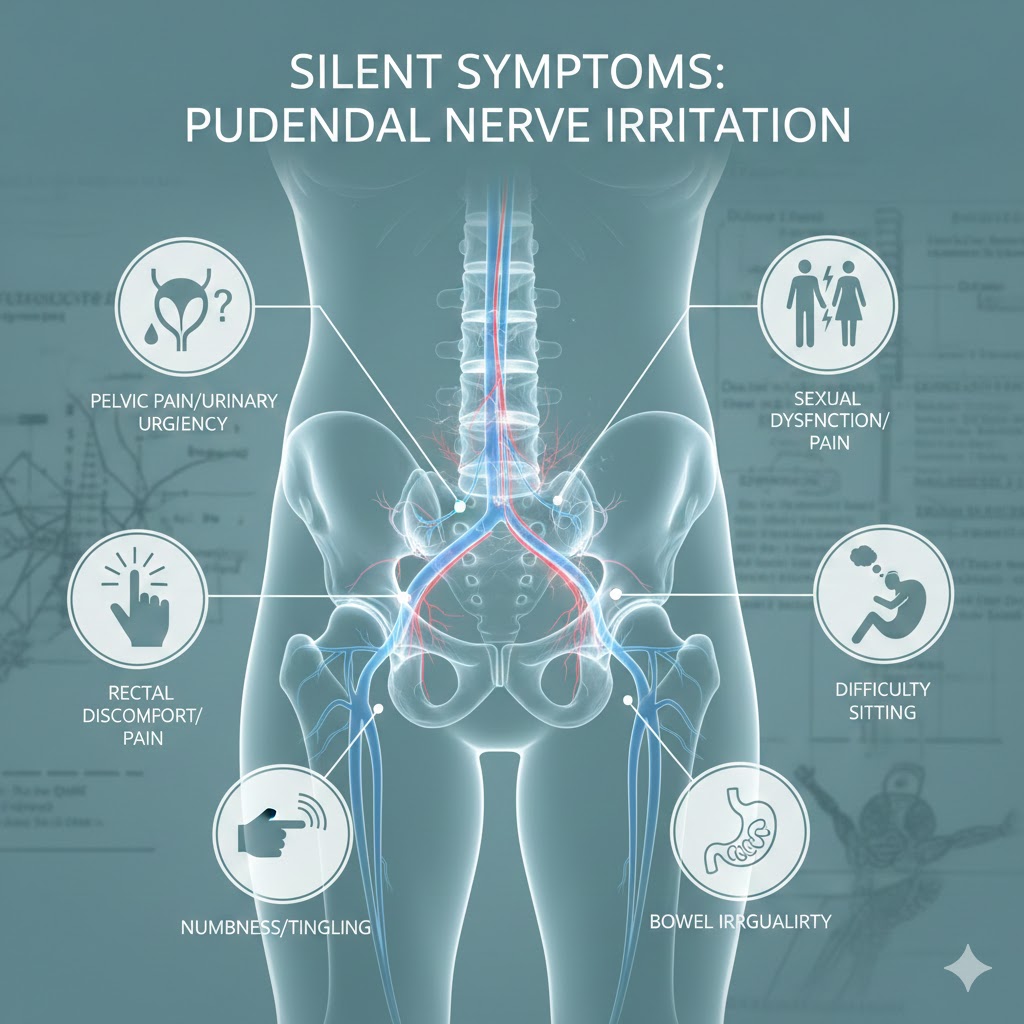
Silent Symptoms That May Indicate Pudendal Nerve Irritation
Below is a complete, detailed list of subtle symptoms that often appear before pain, or in people who never develop pain at all.
1. Strange Genital Sensations Without Pain
Many patients experience abnormal sensations, but no actual pain. These include:
• Tingling or “pins and needles”
A light electric sensation in:
- Penis or clitoris
- Labia
- Scrotum
- Perineum
Often mistaken for circulation issues.
• Numbness or reduced sensitivity
This is one of the most common silent symptoms. People describe it as:
- “I feel less sensation than before.”
- “It feels like the area is asleep.”
- “Something is off.”
• Warmth or mild burning
Not painful—just a warm or “irritated” feeling.
• Crawling or vibration sensations
Some patients describe a feeling similar to:
- A buzzing phone
- A small vibration
- A crawling insect
These sensations often come from nerve irritation, not muscle or skin issues.
2. Mild Pelvic Floor Tightness or Discomfort
The pudendal nerve runs through the pelvic floor muscles. If the nerve becomes irritated, the muscles may tighten to protect it—creating subtle symptoms.
• Feeling of internal tightness
Often described as:
- Pressure
- “Closed” feeling
- Tension that doesn’t relax
• Difficulty relaxing during bowel movements
This may appear long before any noticeable pain.
• A sensation of sitting on a small object
Even without pain, many patients feel:
- A pebble feeling
- A folded cloth
- A small lump under the pelvis
This is a classic early sign of pudendal nerve irritation.
3. Urinary Symptoms That May Be Misdiagnosed
Often mistaken for:
- Urinary tract infections (UTIs)
- Prostatitis
- Interstitial cystitis
- Overactive bladder
But actually caused by pudendal nerve irritation.
• Frequent urination with no infection
You feel the need to urinate often, but:
- Tests come back normal
- No burning during urination
- Bladder feels “irritated”
• Difficulty starting urination
A subtle version of urinary hesitancy:
- You stand or sit, but the flow doesn’t start right away
- No pain—just delay
• Feeling like the bladder didn’t empty fully
Even when it did.
• Dribbling or light leakage
Because the pudendal nerve controls urinary sphincter muscles.
4. Bowel Symptoms Not Recognized as Neurological
Because the pudendal nerve controls the anal sphincter, irritation may cause:
• Hard-to-explain constipation
Not caused by diet—caused by pelvic floor tension.
• A sensation of incomplete evacuation
You finish a bowel movement but feel something is still inside.
• Mild fecal smearing
Tiny traces of stool in underwear—not because of hygiene, but due to:
- Weak sphincter closure
- Delayed nerve signaling
This symptom is one of the most overlooked in early pudendal neuropathy.
5. Sexual Function Changes (Without Pain)
Because the pudendal nerve controls orgasm, arousal, and sensitivity, early silent symptoms often involve sexual function.
• Reduced sensitivity
A common early sign for both men and women.
• Difficulty reaching orgasm
Men may describe weaker sensations; women may describe:
- Orgasm delay
- Weak orgasms
- Loss of satisfaction
• Changes in arousal response
Including:
- Slower arousal
- “Disconnected” feeling
- Lack of genital sensation
• Premature ejaculation or delayed ejaculation
This occurs because nerve signals become irregular.
6. Sitting Discomfort Without Actual Pain
Pudendal nerve irritation is commonly triggered by sitting, especially on hard surfaces.
But early symptoms can be extremely mild.
• Feeling slightly uncomfortable after long sitting
Not pain—just a sense that sitting “isn’t right.”
• Better when standing, worse when sitting
A classic early warning sign.
• Sensation of pressure in the perineum
As if the chair presses too much.
7. Symptom Patterns That Come and Go
Pudendal nerve irritation often starts with intermittent symptoms.
• Symptoms appear only after certain activities
Such as:
- Cycling
- Sitting on hard chairs
- Long car trips
- Intense gym workouts
- Heavy lifting
• Symptoms change location
One week:
- Tingling in the penis
Next week: - Urinary urgency
This “moving” nature confuses most doctors, but it’s typical of pudendal nerve irritation.
• Symptoms appear during stress
Pelvic floor tension increases when stressed, irritating the nerve.
8. Sensations in the Buttocks and Lower Back
Because the pudendal nerve passes near other pelvic nerves, irritation can mimic:
• Mild tailbone discomfort
Especially when sitting.
• A feeling of heaviness in the buttocks
Often mistaken for muscle fatigue.
• Groin tightness
Common in people who sit cross-legged or for long periods.
Why Silent Symptoms Should Not Be Ignored
Early irritation can progress
If the underlying cause is not addressed:
- Pelvic floor muscles may become chronically tight
- The nerve may become more compressed
- Symptoms may become painful
Early detection helps prevent worsening.
Silent symptoms offer clues doctors often miss
When you understand them, you can:
- Describe them more clearly
- Seek appropriate care
- Avoid unnecessary treatments
What Causes Pudendal Nerve Irritation?
Most common causes
- Chronic sitting
- Cycling
- Heavy lifting
- Pelvic floor hypertonicity
- Constipation and straining
- Pelvic surgery
- Trauma or falls
- High stress
- Childbirth (for women)
Understanding the cause helps guide recovery.
How Doctors Diagnose Pudendal Nerve Problems
Although diagnosis is often challenging, clinicians may use:
Physical examination
Checking:
- Pelvic floor tension
- Trigger points
- Sensation patterns
MRI or MR Neurography
To rule out major structural issues.
Pudendal nerve block
If a nerve block reduces symptoms, it confirms involvement.
Early Management Tips (Evidence-Based & Simple)
These are general health measures, not medical treatment.
1. Reduce sitting time
Use:
- Cushion
- Standing breaks
- Softer surfaces
2. Improve posture
Sit with:
- Neutral spine
- Relaxed pelvic floor
3. Avoid triggers temporarily
Such as:
- Cycling
- Heavy lifting
4. Gentle pelvic floor relaxation
Diaphragmatic breathing can reduce pelvic tension.
5. See a pelvic floor physiotherapist
A specialist can help identify whether pelvic muscles are contributing.
Medical Sources for Verification
Here are three reputable medical sources discussing pudendal nerve irritation, pelvic pain, and pelvic neuropathy:
- Cleveland Clinic – Pudendal Neuralgia
https://my.clevelandclinic.org/health/diseases/22951-pudendal-neuralgia - Mayo Clinic – Chronic Pelvic Pain Overview
https://www.mayoclinic.org/diseases-conditions/chronic-pelvic-pain - U.S. National Library of Medicine (NIH) – Pelvic neuropathies and pudendal nerve
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3498255/
These references provide scientific background and confirm the symptoms and mechanisms discussed above.
Conclusion
Silent symptoms of pudendal nerve irritation often go unnoticed, misunderstood, or misdiagnosed. By recognizing subtle signs—such as tingling, numbness, urinary changes, mild pelvic tightness, or sitting discomfort—you can identify the condition early and prevent progression. Understanding these early clues empowers you to seek proper evaluation, protect your pelvic health, and avoid years of confusion or unnecessary treatments.
Disclaimer:
This article is for educational purposes only and does not replace professional medical diagnosis, examination, or treatment. Always consult a qualified healthcare provider regarding any health concerns.