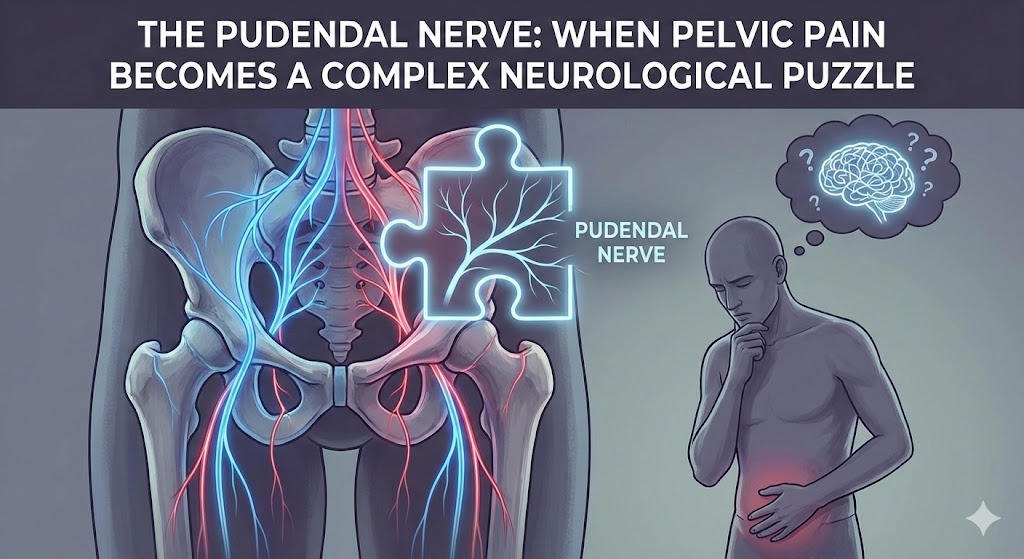
Pelvic pain is one of the most confusing and frustrating conditions a person can experience. Among the many causes, pudendal nerve dysfunction—including irritation, entrapment, or neuropathy—is one of the most misunderstood. Because the pudendal nerve controls essential functions like bladder control, bowel activity, and sexual sensation, its dysfunction can dramatically affect someone’s daily life.
Yet diagnosing pudendal nerve–related pelvic pain remains extremely challenging. Symptoms often overlap with urinary, gynecological, gastrointestinal, orthopedic, and psychological conditions. This is why pudendal nerve pain is frequently called a “complex neurological puzzle.”
This article explains everything clearly and simply—from anatomy to symptoms, causes, diagnosis, modern treatments, and long-term management—with a strong focus on accuracy, search engine optimization, and user-friendly explanations.
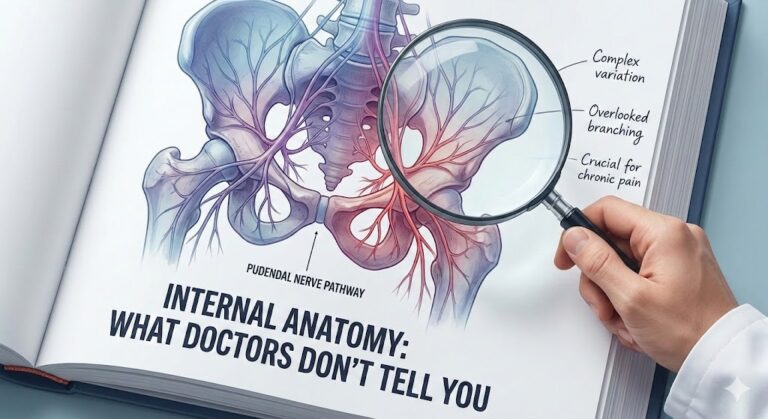
Understanding the Pudendal Nerve
Where the Pudendal Nerve Is Located
The pudendal nerve is one of the major nerves in the pelvis. It:
- originates from the sacral nerve roots S2, S3, and S4
- travels through the greater sciatic foramen
- loops around a ligament
- enters the pelvis again through the lesser sciatic foramen
- passes through the Alcock’s canal (a narrow tunnel in the pelvis)
Along this route, the nerve divides into three branches:
- Inferior rectal nerve — controls the anal sphincter
- Perineal nerve — sensation to the perineum and motor supply to pelvic floor muscles
- Dorsal nerve of the penis or clitoris — responsible for sexual sensation
This long, narrow, curved path makes the pudendal nerve vulnerable to irritation or compression.
What Makes Pudendal Nerve Pain So Complex?
1. It Mimics Many Other Conditions
Pudendal nerve pain can be mistaken for:
- urinary tract infections
- prostatitis
- endometriosis
- pelvic floor dysfunction
- hemorrhoids
- vulvodynia
- coccyx injury
- sciatica
Because symptoms overlap with so many systems, people often see multiple specialists before receiving a correct diagnosis.
2. Symptoms Come from Several Body Systems at Once
The pudendal nerve affects:
- bladder function
- bowel control
- sexual sensation
- pelvic floor muscles
That means one irritated nerve can create symptoms across multiple areas, making the picture confusing.
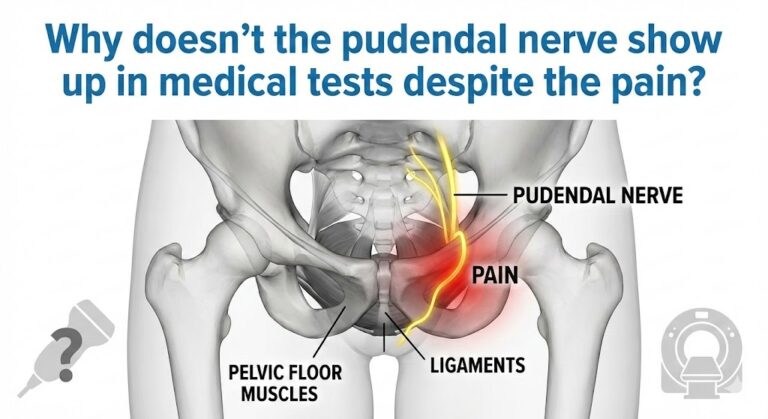
3. Standard Imaging Often Looks “Normal”
MRI or CT scans often fail to show pudendal nerve problems because the nerve is small and hidden between deep pelvic structures.
4. The Pelvic Floor Adds Another Layer of Complexity
Tight, overactive, or weak pelvic floor muscles can irritate the pudendal nerve even without structural entrapment.
Pain may be both muscular and neurological, which complicates treatment.
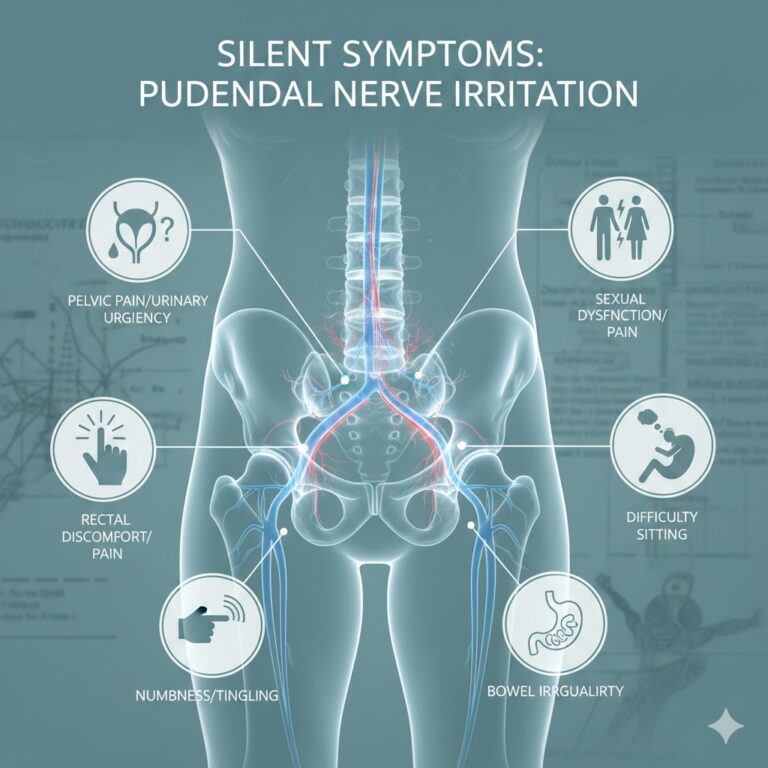
Symptoms of Pudendal Nerve Irritation or Entrapment
Common Symptoms
People may experience:
- burning, stabbing, or electric-like pelvic pain
- pain while sitting, especially on hard surfaces
- pain relieved when standing or lying down
- genital numbness or hypersensitivity
- a feeling of a “foreign object” in the rectum or vagina
- urinary urgency or frequency
- difficulty emptying the bladder
- constipation or difficulty with bowel movements
- sexual dysfunction (difficulty with arousal or painful arousal)
These symptoms vary widely depending on which branch of the nerve is affected.
Pain While Sitting: A Key Indicator
One of the hallmark signs is pain when sitting, especially if it improves when standing or sitting on a toilet seat (which removes pressure from the nerve).
Symptoms Are Often One-Sided
Most cases affect only one side of the pelvis, though both sides can be affected in some individuals.
Causes: Why the Pudendal Nerve Becomes Irritated
Mechanical or Physical Compression
The nerve may become compressed due to:
- prolonged sitting (drivers, office workers, cyclists)
- heavy lifting
- childbirth trauma
- pelvic surgeries
- direct injury or fall onto the buttocks
- tight pelvic floor muscles
- chronic constipation
Pudendal Neuralgia vs. Pudendal Entrapment
They are not the same condition:
- Pudendal Neuralgia: irritation or dysfunction of the nerve
- Pudendal Entrapment: the nerve is physically trapped or compressed along its path
Entrapment is less common but more severe.
Pelvic Floor Dysfunction as a Major Contributor
Overactive (tight) pelvic floor muscles can compress the pudendal nerve, causing:
- burning
- pressure
- radiating pain
- trouble relaxing the bladder
In these cases, pelvic floor physical therapy is highly effective.
Posture and Lifestyle Factors
Poor posture, especially slouching while sitting, can put pressure on the pelvic outlet and irritate the nerve.
How Pudendal Nerve Problems Are Diagnosed
Diagnosis involves several steps because no single test provides absolute confirmation.
1. Detailed Medical History
Doctors analyze:
- symptom location
- symptom triggers
- sitting tolerance
- urinary and bowel habits
- pain patterns
2. Physical Examination
A specialized pelvic examination evaluates:
- pelvic floor muscle tone
- trigger points
- nerve sensitivity
- musculoskeletal alignment
3. Diagnostic Nerve Blocks
A pudendal nerve block involves injecting a small amount of anesthetic near the nerve.
If pain temporarily improves, this strongly suggests the pudendal nerve is involved.
4. MRI of the Pelvis
While MRI cannot always “prove” pudendal nerve entrapment, it can:
- rule out tumors
- identify structural abnormalities
- confirm surrounding muscle or ligament issues
5. Electromyography (EMG)
EMG may help detect nerve dysfunction, although results are not always definitive.
Treatment Options: A Multi-Layered Approach
Pudendal nerve problems are best treated using multiple strategies at once.
Pelvic Floor Physical Therapy
This is one of the most effective treatments, especially for muscle-based problems.
Therapy may include:
- muscle relaxation techniques
- biofeedback
- trigger point release
- myofascial techniques
- stretching
- posture correction
It is essential to work with a specialist physiotherapist, not general therapy.
Lifestyle Modifications
1. Sit Less, Move More
Standing breaks every 20–30 minutes reduce nerve pressure.
2. Use a Pressure-Relief Cushion
Donut cushions are not ideal. A U-shaped or T-shaped cushion is better because it removes pressure from the perineum.
3. Avoid Activities That Irritate the Nerve
For example:
- cycling
- horseback riding
- heavy squats
- prolonged sitting in cars
Medications
Doctors may prescribe medications to calm nerve irritation, such as:
- anti-inflammatory medications (for short-term use)
- neuropathic pain modifiers (e.g., gabapentin, pregabalin, amitriptyline)
- muscle relaxants (for pelvic floor tension)
These should always be taken under medical supervision.
Pudendal Nerve Blocks
Nerve blocks can reduce inflammation and interrupt pain signaling.
They may be used:
- diagnostically
- therapeutically (series of injections)
Some patients experience significant long-term relief.
Radiofrequency Ablation (RFA)
In selected cases, pulsed radiofrequency treatment can calm the nerve without destroying it.
Psychological Support
Chronic pelvic pain can create emotional stress.
Cognitive behavioral therapy (CBT) or counseling may help improve:
- coping
- sleep
- anxiety related to symptoms
This does not mean pain is “in your head”—rather, the brain and nerves are deeply connected.
Surgical Options
Surgery is considered only when:
- symptoms strongly indicate entrapment
- conservative treatments fail
- diagnostic nerve blocks support the diagnosis
Surgery aims to decompress the nerve, but results vary and require a specialist surgeon.
Long-Term Management and Recovery
Recovery from pudendal nerve problems is often gradual.
People typically improve over months, not weeks.
Key Principles for Recovery
- Be consistent with pelvic floor therapy
- Avoid irritating activities
- Use proper sitting cushions
- Practice deep breathing and relaxation
- Improve posture and core stability
- Address constipation or urinary strain
The Importance of Patience
Nerves heal slowly—often 1–3 millimeters per day.
Most individuals improve significantly with conservative therapy.
Can Pudendal Nerve Pain Be Prevented?
While not all cases are preventable, risk can be reduced by:
- avoiding prolonged sitting
- using ergonomic chairs
- maintaining good posture
- avoiding excessive cycling without proper seat adjustment
- strengthening the core and hips
- preventing chronic constipation
- treating pelvic muscle tension early
When to See a Doctor
Seek medical help if you experience:
- pelvic pain that worsens when sitting
- changes in bladder or bowel habits
- unexplained genital numbness
- burning or electric sensations in the pelvis
- pain lasting more than a few weeks
Early evaluation improves outcomes dramatically.
Reliable Medical Sources
Here are three trusted references for further reading:
- Mayo Clinic — Pudendal Neuralgia Overview
https://www.mayoclinic.org/ - Cleveland Clinic — Pelvic Floor & Pudendal Nerve Disorders
https://my.clevelandclinic.org/ - National Center for Biotechnology Information (NCBI) — Research Articles on Pudendal Neuralgia
https://www.ncbi.nlm.nih.gov/
Conclusion
Pudendal nerve–related pelvic pain is a complex condition that involves neurological, muscular, and biomechanical components. Its symptoms are often confusing and can imitate many other disorders, which explains why diagnosis is frequently delayed.
However, with modern evaluation techniques, specialized pelvic therapy, lifestyle adjustments, and targeted medical treatments, most people can achieve meaningful improvement and return to a healthier, more comfortable life.
Disclaimer:
This article is for educational purposes only and does not replace professional medical advice. Always consult a qualified healthcare provider for diagnosis or treatment.