Why Focus on the Pudendal Nerve?
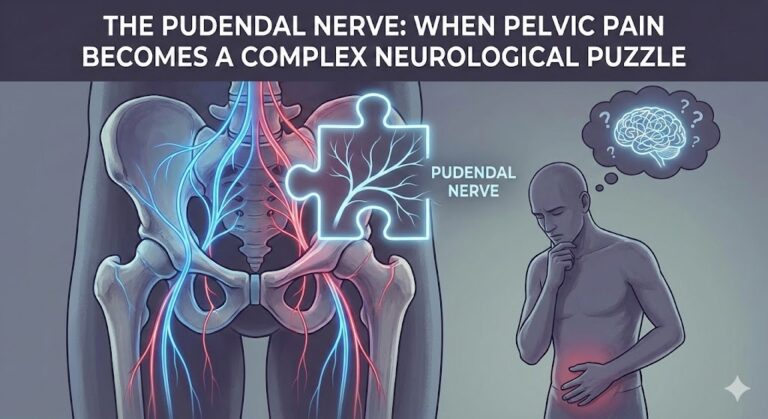
The pudendal nerve is one of the most critical peripheral nerves in the pelvic and perineal region. Yet, many patients and even some physicians are unaware of its internal pathway, branches, and intricate anatomical relationships that can affect function or cause syndromes such as pudendal neuralgia.
Understanding “what doctors don’t tell you” is essential because neglecting detailed anatomy can lead to misdiagnosis, delayed treatment, or complications after surgeries. This article aims to provide an in-depth, evidence-based analysis to fill this knowledge gap.
Origin and Course of the Pudendal Nerve
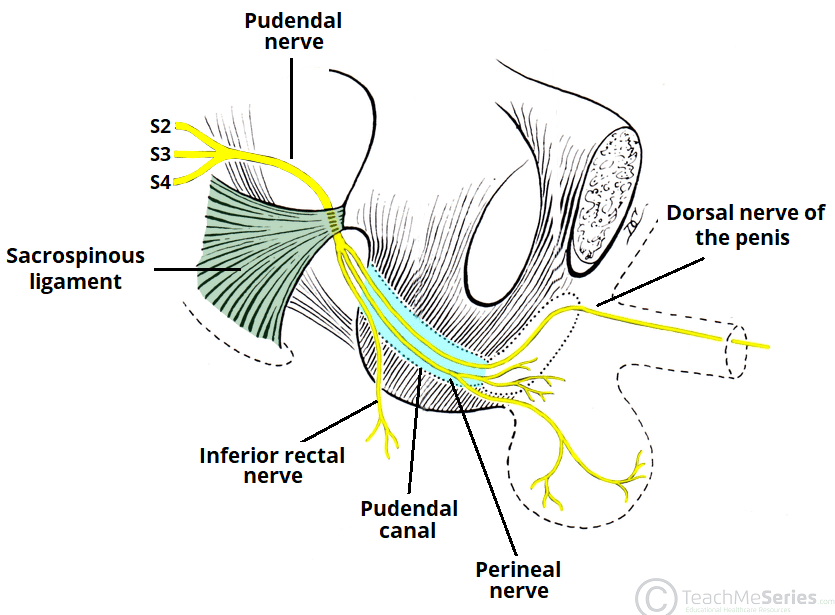
- Nerve Roots: The pudendal nerve arises from the ventral rami of S2, S3, and S4 spinal nerves (TeachMeAnatomy).
- Sacral Plexus Position: It is part of the sacral plexus located on the posterior wall of the pelvis. From here, the nerve descends toward the lower pelvis (NCBI Bookshelf).
- Exiting the Pelvis: It exits through the greater sciatic foramen, passing near the ischial spine, between the sacrospinous and sacrotuberous ligaments, before re-entering the pelvis via the lesser sciatic foramen (TeachMeAnatomy).
- Alcock’s Canal: Inside the pelvis, it runs anteriorly with the internal pudendal artery and vein within Alcock’s canal, a fibrous tunnel formed by the obturator internus fascia (TeachMeAnatomy).
- Branches within the Canal: The nerve gives off the inferior rectal nerve, perineal nerve, and continues as the dorsal nerve of the penis or clitoris (TeachMeAnatomy).
Important Note: There is considerable anatomical variation between individuals in the nerve’s course and branches. Understanding this variation is critical for clinical practice (PubMed).
Motor and Sensory Functions
Motor Function
- The perineal branch innervates pelvic floor muscles such as bulbospongiosus, ischiocavernosus, and parts of the levator ani (puborectalis, pubococcygeus, iliococcygeus) (TeachMeAnatomy).
- The inferior rectal nerve controls the external anal sphincter and external urethral sphincter, essential for voluntary bowel and bladder control (TeachMeAnatomy).
Sensory Function
- Provides sensation to the skin around the perineum, vulva, scrotum, and anus (TeachMeAnatomy).
- The dorsal nerve of the penis or clitoris mediates sexual sensation, including arousal and erection (TeachMeAnatomy).
Thus, the pudendal nerve has a dual role: motor control of pelvic floor muscles and sensory perception in the genital and perineal region.
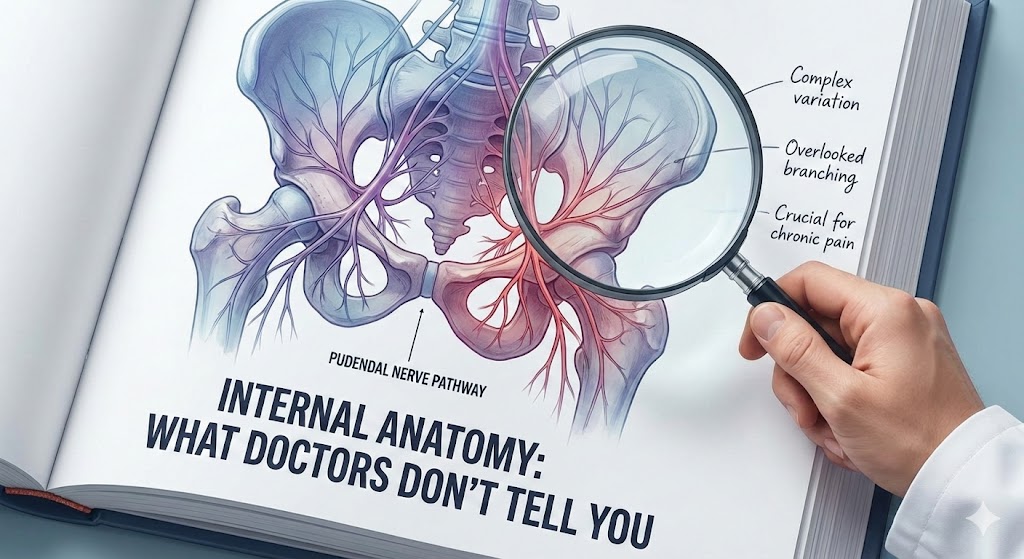
Anatomical Variations and Their Significance
One of the key things “doctors often don’t tell you” is that anatomy is not uniform. Recent anatomical and imaging studies reveal:
- Variations in the nerve’s relation to the sacrospinous and sacrotuberous ligaments (PubMed).
- The inferior rectal nerve may branch earlier in some individuals, meaning sites of nerve entrapment differ.
- Such variations influence surgical risks, likelihood of neuralgia, and effectiveness of nerve blocks (PubMed).
Therefore, relying solely on a “standard anatomy map” can be misleading. Each patient may have a unique nerve pathway.
Why Doctors Often Don’t Explain These Details
Several reasons explain the lack of detailed discussion:
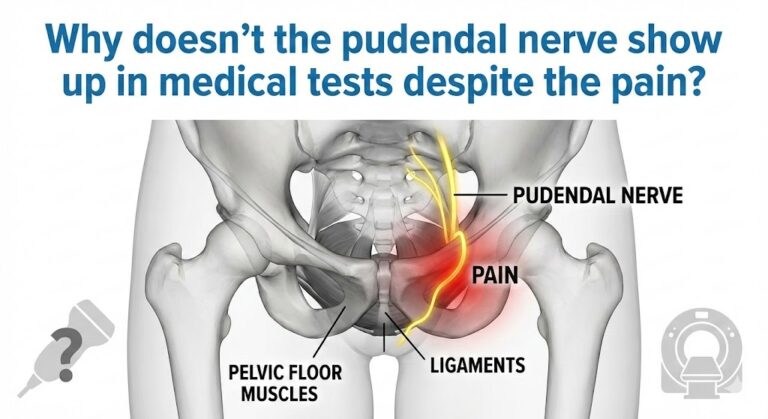
- Focus on Symptoms: Physicians often prioritize symptom management over anatomical minutiae.
- Training Gaps: Not all physicians, particularly non-specialists, are trained in detailed pelvic nerve variations.
- Difficulty in Diagnosis: Branching variations can only be seen through dissection or advanced imaging, rarely required in routine care.
- Surgical Risk: Lack of knowledge about variations increases risk of iatrogenic injury.
Clinical Implications: When Detailed Knowledge Matters
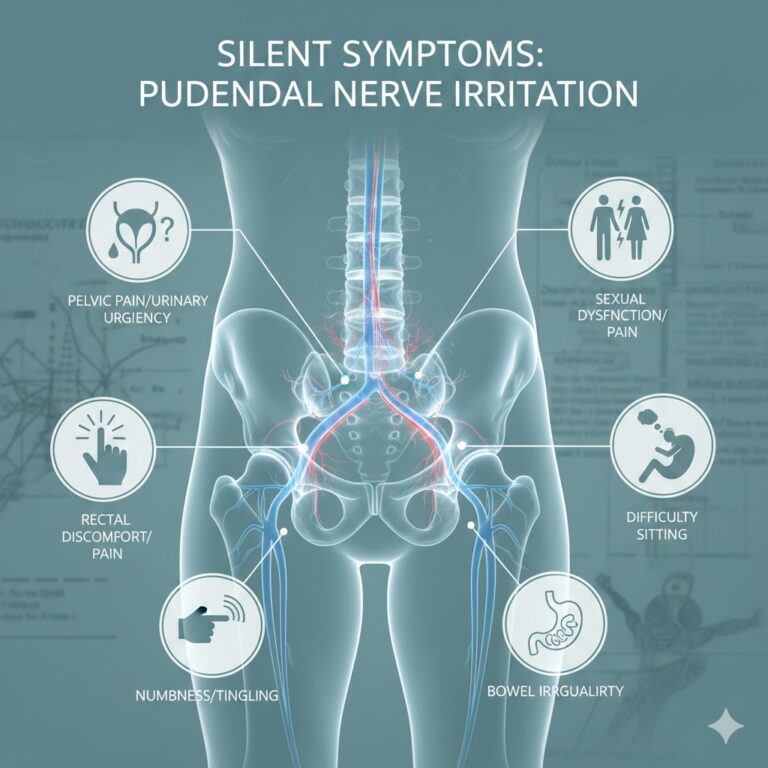
Pudendal Neuralgia or Nerve Entrapment
- Variations make the nerve susceptible to compression at unexpected points (e.g., ischial spine, Alcock’s canal) (PubMed).
- Entrapment can cause chronic perineal pain, numbness, sitting discomfort, sexual dysfunction, or incontinence (PubMed).
Surgery and Pelvic Procedures
- Pelvic, anal, or urogenital surgeries risk injuring the nerve if variations are not considered (NCBI Bookshelf).
- Accurate anatomical knowledge is essential for nerve blocks, neurolysis, and rehabilitation (PubMed).
Physical Therapy and Pelvic Floor Rehabilitation
- Nerve compression can mimic muscular weakness; exercises alone may fail without addressing neural causes.
- Integrating nerve assessment with therapy improves outcomes.
Common Mistakes Due to Ignoring Detailed Anatomy
- Assuming the nerve has a fixed anatomical path — ignoring patient-specific variation.
- Neglecting Alcock’s canal and associated vessels during interventions.
- Overlooking minor branches that may be clinically significant.
- Not using imaging for unexplained symptoms.
- Failing to inform patients that anatomy can vary individually, leading to misunderstandings.
Latest Research Insights
The 2024 pictorial review “Anatomy of the pudendal nerve in clinically important areas” analyzed modern anatomical studies and confirmed:
- Significant variation in branching patterns.
- Early branching of the inferior rectal nerve occurs in some individuals, explaining variable symptoms.
- Understanding these patterns is crucial for surgeons, pain specialists, urologists, and gynecologists to prevent iatrogenic injury (PubMed).
Educational sources like TeachMeAnatomy provide accurate maps of sensory and motor branches (TeachMeAnatomy).
Importance of Detailed Anatomy Awareness
- For Practitioners: Ensures safe planning of surgeries, interventions, or nerve blocks.
- For Patients: Explains why some treatments fail and encourages comprehensive evaluation.
- For Researchers: Highlights the need for large-sample anatomical studies due to individual variation.
Recommendations to Reduce Risk of Nerve Injury
- Use image-guided techniques for nerve blocks or injections.
- Surgeons should be trained in anatomical variations; plan surgeries meticulously.
- Consider nerve compression in chronic symptoms, not just muscular weakness.
- Combine pelvic floor therapy with diagnostic imaging when necessary.
- Educate patients that anatomy can vary individually.
Conclusion
The pudendal nerve is far more than a simple pelvic nerve; it is a vital structure traveling through complex pathways, accompanied by vessels, and branching into intricate motor and sensory components. Individual anatomical variation is significant, yet often overlooked by both clinicians and patients. Ignorance or neglect of these details can result in misdiagnosis, post-surgical complications, or failed therapies.
Modern anatomical studies emphasize patient-specific evaluation as essential for effective treatment, risk reduction, and optimal outcomes.
Reliable Medical Sources
- Anatomy, Abdomen and Pelvis, Pudendal Nerve — StatPearls (NCBI Bookshelf)
- The Pudendal Nerve — TeachMeAnatomy (TeachMeAnatomy)
- Anatomy of the pudendal nerve in clinically important areas: a pictorial essay and narrative review (2024) (PubMed)
Disclaimer
This article provides general anatomical and medical information for educational purposes. It does not replace professional medical advice. For diagnosis, treatment, or management of symptoms, consult a qualified healthcare professional specializing in neurology, urology, or pelvic medicine.