Why the PSA Test Matters, and When Men Should Consider It
The Prostate-Specific Antigen (PSA) test is a simple blood test that measures the level of PSA protein in the bloodstream. It is widely used as an early-detection tool for prostate conditions such as prostatitis, benign enlargement, and most importantly—prostate cancer. However, the PSA test is not perfect: elevated levels do not automatically mean cancer, and normal levels do not fully rule it out.
Therefore, the question “When should a man check his prostate?” requires a careful balance between the benefits of early detection and the risks of unnecessary interventions.
This comprehensive, search-optimized article explains who needs PSA testing, when, why, and how, following the latest global medical guidelines and backed by reliable scientific sources.
What Is the PSA Test and How Does It Work?
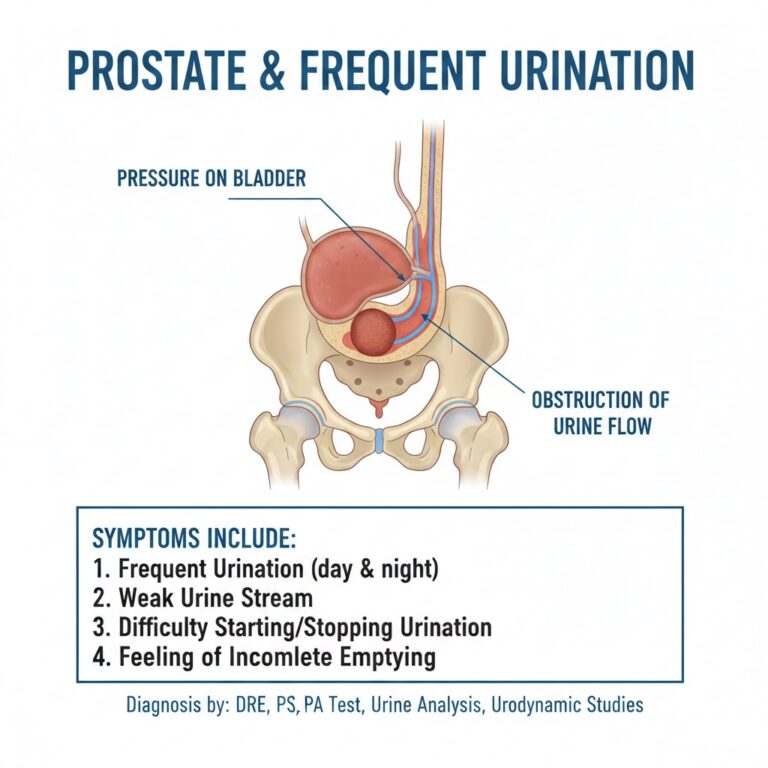
PSA is a protein produced by cells of the prostate gland. When the prostate becomes enlarged, inflamed, or affected by disease, more PSA leaks into the bloodstream.
The PSA test measures this concentration in nanograms per milliliter (ng/mL).
A single result is not enough for a diagnosis; it must be interpreted alongside:
- Age
- Family history
- Digital rectal examination (DRE)
- Medication use
- Recent sexual activity or urinary infections
All of which can alter PSA levels.
Why PSA Alone Is Not Enough
Although PSA is sensitive, it is not perfectly specific.
High PSA does not always mean cancer; it may result from:
- Benign prostate enlargement
- Prostatitis
- Recent ejaculation
- Urinary tract infection
This leads to false positives, extra imaging, biopsies, and anxiety.
On the other hand, some aggressive prostate cancers may show only a mild PSA rise in early stages.
Therefore, modern guidelines recommend a risk-adapted screening approach and shared decision-making between patient and doctor.
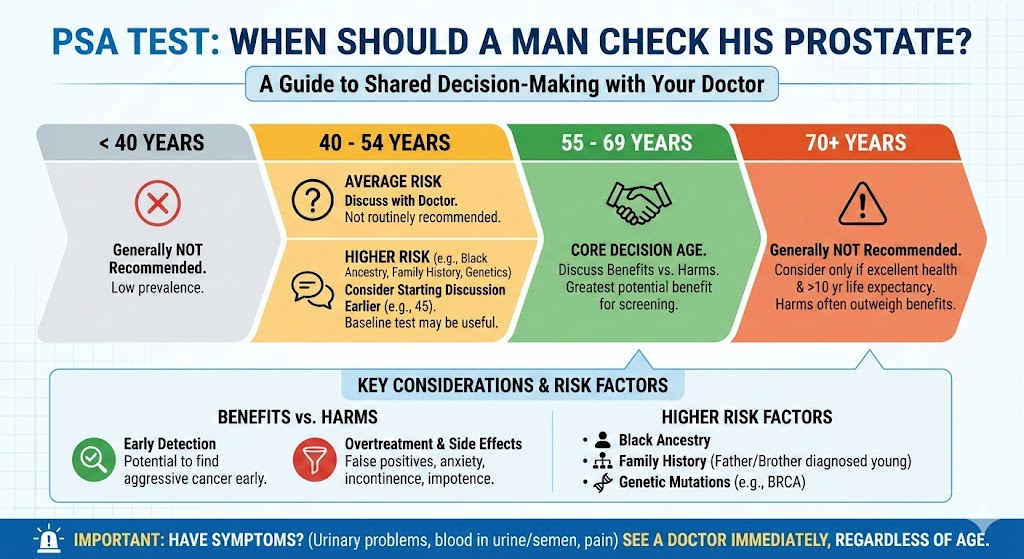
Who Is Considered High-Risk and Should Start PSA Testing Earlier?
Some men are at higher risk of developing prostate cancer, especially at a younger age.
You should consider early PSA screening (age 40–45) if you have:
1. A first-degree relative (father, brother) diagnosed with prostate cancer before age 65.
2. Genetic mutations, such as BRCA1 or BRCA2.
3. African ancestry, which carries significantly higher risk and more aggressive disease patterns.
For these groups, the conversation about PSA testing should begin much earlier than for the general population.
When Should Average-Risk Men Begin PSA Testing?
Recommendations vary slightly across organizations, but the global consensus is:
Ages 55–69
Men in this age range should discuss PSA screening with their doctor.
Screening every 2–4 years may be beneficial.
Ages under 55 but above 40
Testing may be recommended if moderate/high-risk factors exist.
Ages 70 and above
Many guidelines recommend against routine screening after age 70, unless life expectancy is good and specific reasons justify continued testing.
A Practical Timeline: When to Start and How Often to Repeat PSA Testing
Modern strategies are shifting toward baseline PSA testing:
Baseline PSA at age 40–50
If PSA is:
- Below 1.0–1.5 ng/mL → Very low risk: repeat in 5–8 years
- Between 1.5–3 ng/mL → Medium risk: test every 2 years
- Above 3 ng/mL → Requires further evaluation (repeat test, DRE, MRI, possible biopsy)
These ranges follow recent European and American urology guidelines and large research trials.
Benefits of Early PSA Testing
When used correctly, PSA testing may:
- Detect treatable cancers before they spread
- Reduce prostate cancer deaths in selected groups
- Offer men more treatment options at earlier stages
However, the true benefit depends on choosing the right men for screening and avoiding unnecessary treatment for low-risk disease.
Risks and Side Effects of PSA Screening
PSA screening is not risk-free:
1. False positives
Can lead to:
- Anxiety
- MRI scans
- Biopsies
- Possible infections or bleeding
2. Overdiagnosis
Detecting slow-growing cancers that may never cause harm.
This often leads to overtreatment, with side effects such as:
- Urinary issues
- Erectile dysfunction
- Surgical or radiation complications
For this reason, PSA screening must be a shared decision.
How Doctors Interpret PSA Levels: A Practical Explanation
Doctors evaluate PSA results using several factors:
1. PSA absolute value
The raw number measured.
2. PSA velocity (rate of change)
Rapid increases may indicate a problem.
3. Free-to-total PSA ratio
Useful in distinguishing benign causes from cancer.
4. Digital rectal exam (DRE)
Checks prostate size, shape, and surface.
5. MRI imaging (mpMRI)
Provides highly accurate visualization before deciding on a biopsy.
In many cases, when PSA is high, doctors repeat the test after excluding temporary causes such as infection or recent ejaculation.
Modern Tools That Improve PSA Accuracy
To avoid unnecessary biopsies, doctors now use:
1. Risk-prediction calculators
Combine PSA, age, and family history.
2. Multiparametric MRI (mpMRI)
Used before biopsy to target suspicious areas.
3. Advanced biomarkers
Offered in specialized centers to refine risk assessment.
These tools significantly reduce unnecessary procedures.
A Practical Checklist for Men Considering PSA Testing
Before you decide, follow these steps:
- Discuss your family history and risk level with a clinician.
- Understand the potential harms of false positives and unnecessary biopsies.
- Start earlier (40–45) if you are high-risk (family history, genetics, African ancestry).
- Avoid ejaculation for 48 hours before testing.
- Repeat the test before moving to biopsy if results are unexpectedly high.
Frequently Asked Questions (FAQ)
Is PSA a test only for cancer?
No. It rises with many prostate conditions, not only cancer.
Do I need PSA screening every year?
Not necessarily. Every 2–4 years is enough for most men who choose screening.
What is a normal PSA level?
There is no universal cutoff, but traditionally <4 ng/mL was considered “normal.”
Modern guidelines focus more on age-specific and risk-specific ranges rather than one fixed number.
What Changed in Recent Guidelines?
The major shift is moving from routine annual screening to risk-adapted screening, because:
- Annual PSA caused too many false alarms
- Many harmless cancers were treated aggressively
- Modern MRI and biomarkers reduce unnecessary biopsies
The new approach improves accuracy and minimizes harm.
Trusted Medical Sources (required 3 links)
These are authoritative sources used by clinicians worldwide:
- European Association of Urology (EAU) Guidelines
https://uroweb.org/guidelines - American Urological Association (AUA) — Early Detection Guidelines
https://www.auanet.org/guidelines - Centers for Disease Control and Prevention (CDC) — Prostate Cancer Screening
https://www.cdc.gov/cancer/prostate/
Making the Right Decision
There is no one-size-fits-all answer to when a man should check his prostate.
The decision depends on:
- Age
- Family history
- Genetic risks
- Personal preferences
- Expected benefits versus harms
For most men:
- Begin the discussion at age 55–69
- High-risk men start at age 40–45
- Screening intervals of 2–4 years are usually enough
Using modern tools like MRI and risk calculators makes PSA screening safer and more accurate.
Disclaimer
This article is for educational purposes only and does not replace professional medical advice. Always consult a qualified physician before making any medical decisions or undergoing testing.