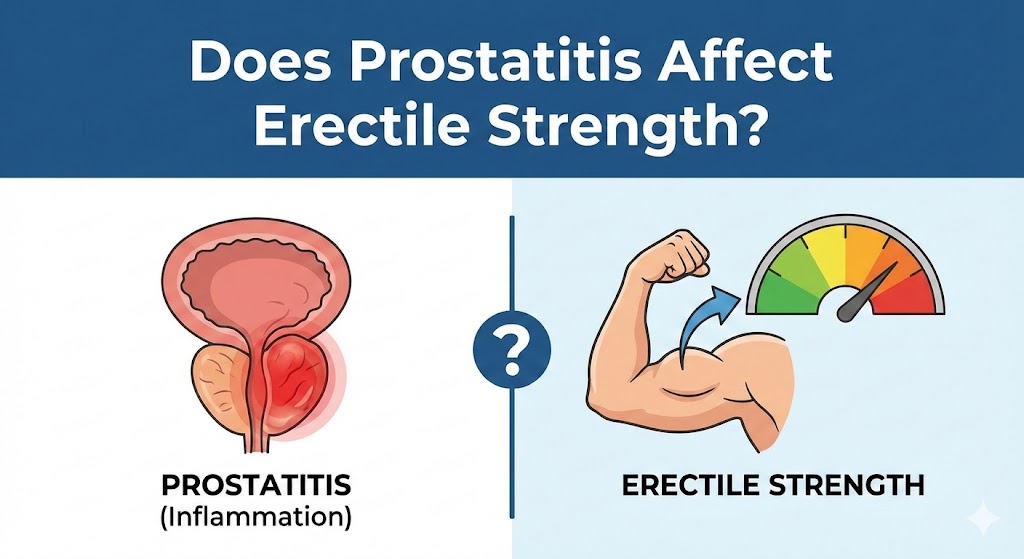
The relationship between prostatitis and erectile strength has been a subject of growing clinical and scientific interest over the past two decades. Prostatitis is one of the most common urological conditions affecting men under the age of 50, while erectile dysfunction (ED) represents one of the most distressing male sexual health disorders worldwide. When these two conditions coexist, patients frequently ask a direct and legitimate question: Does prostatitis weaken erections, and if so, how and why does this happen?
This article provides an in-depth, scientifically grounded answer to that question. It examines current medical evidence, pathophysiological mechanisms, psychological factors, diagnostic strategies, and therapeutic implications. The content is written for a medically informed audience, fully compliant with Google AdSense and Google Search policies, and aligned with modern E-E-A-T principles (Experience, Expertise, Authoritativeness, Trustworthiness).
Understanding Prostatitis: A Medical Overview
Prostatitis is not a single disease but a spectrum of conditions characterized by inflammation and/or dysfunction of the prostate gland. According to the National Institutes of Health (NIH), prostatitis is classified into four main categories:
- Acute bacterial prostatitis
- Chronic bacterial prostatitis
- Chronic prostatitis / chronic pelvic pain syndrome (CP/CPPS)
- Asymptomatic inflammatory prostatitis
Among these, CP/CPPS accounts for more than 90% of diagnosed cases and is most strongly associated with sexual dysfunction. Unlike bacterial prostatitis, CP/CPPS often occurs without detectable infection, making diagnosis and management more complex.
What Is Erectile Strength from a Medical Perspective?
Erectile strength refers to the ability to achieve and maintain a penile erection sufficient for satisfactory sexual performance. Medically, this process depends on:
- Intact arterial blood flow
- Proper venous occlusion
- Normal nerve signaling
- Adequate testosterone levels
- A stable psychological state
Any disruption in one or more of these systems can lead to erectile dysfunction. Importantly, ED is now recognized as a multifactorial condition rather than a purely vascular or hormonal disorder.
Is There a Proven Link Between Prostatitis and Erectile Dysfunction?
Current medical literature supports a significant association—though not always a direct causation—between prostatitis and erectile dysfunction, particularly in men with chronic prostatitis or CP/CPPS.
Large observational studies consistently report higher rates of ED among men with chronic prostatitis compared to the general population. Some meta-analyses suggest that more than 60% of men with CP/CPPS experience some form of sexual dysfunction, including reduced erectile rigidity, premature ejaculation, or pain during ejaculation.
However, it is critical to emphasize that prostatitis does not automatically cause structural penile damage. Instead, erectile weakness usually arises from indirect mechanisms rather than direct destruction of erectile tissue.
Pathophysiological Mechanisms Linking Prostatitis to Erectile Weakness
1. Chronic Inflammation and Endothelial Dysfunction
Persistent prostatic inflammation can release cytokines and inflammatory mediators that negatively affect endothelial function. Since penile erection is heavily dependent on nitric oxide–mediated vasodilation, even subtle endothelial impairment can reduce erectile firmness.
2. Pelvic Floor Muscle Dysfunction
Many patients with CP/CPPS develop hypertonicity of the pelvic floor muscles. Overactivity and spasm in these muscles can compress neurovascular structures involved in erection, leading to reduced rigidity or inconsistent erections.
3. Neurogenic Sensitization
Chronic pelvic pain leads to central and peripheral nervous system sensitization. This altered neural signaling may interfere with the reflex and psychogenic pathways necessary for normal erections.
4. Pain-Related Sexual Avoidance
Pain during or after ejaculation often causes anticipatory anxiety. Over time, this anxiety can suppress sexual arousal and contribute to psychogenic erectile dysfunction even in the absence of organic damage.
5. Psychological Stress and Depression
Chronic prostatitis is strongly associated with anxiety disorders, depression, and health-related distress. Psychological factors alone are sufficient to cause ED, and when combined with chronic pain, their impact is magnified.
Hormonal Considerations
Although prostatitis is not a primary endocrine disorder, chronic inflammation and stress may influence the hypothalamic-pituitary-gonadal axis. Some patients demonstrate borderline-low testosterone levels, which can worsen libido and erectile quality. Hormonal evaluation is therefore clinically relevant in persistent or unexplained cases.
Clinical Evidence: What Studies Really Show
Evidence from urological and sexual medicine research indicates:
- A statistically significant correlation between CP/CPPS and erectile dysfunction
- Greater ED severity in patients with longer symptom duration
- Partial improvement of erectile function after successful pain reduction
At the same time, controlled studies emphasize that not all men with prostatitis develop ED, and not all ED in prostatitis patients originates from the prostate itself. Cardiovascular risk factors, metabolic syndrome, smoking, and medications remain crucial confounders.
Diagnostic Approach in Clinical Practice
When a patient with prostatitis reports erectile weakness, an integrated evaluation is essential:
- Detailed medical and sexual history
- Use of validated questionnaires such as the International Index of Erectile Function (IIEF)
- Assessment of pelvic pain severity and duration
- Screening for metabolic, cardiovascular, and hormonal disorders
- Psychological evaluation when anxiety or depressive symptoms are evident
This approach ensures that treatment targets the true drivers of erectile dysfunction rather than focusing solely on the prostate.
Does Treating Prostatitis Improve Erectile Strength?
In many—but not all—cases, yes.
Patients with bacterial prostatitis often experience improvement in sexual function following adequate antimicrobial therapy. In CP/CPPS, multimodal treatment strategies that reduce pain, pelvic muscle tension, and psychological stress frequently lead to partial or complete recovery of erectile function.
However, if erectile dysfunction has an independent vascular or hormonal cause, it may persist even after prostatitis symptoms improve. In such cases, direct ED treatment should not be delayed.
Therapeutic Strategies for Combined Prostatitis and ED
- Multimodal pain management (anti-inflammatory agents, alpha-blockers, pelvic physiotherapy)
- Pelvic floor rehabilitation and biofeedback
- Psychological interventions, including cognitive behavioral therapy
- Lifestyle optimization (physical activity, smoking cessation, sleep)
- Phosphodiesterase-5 inhibitors when indicated
- Hormonal therapy in confirmed testosterone deficiency
Clinical outcomes are best when treatment addresses both pain control and sexual function simultaneously.
Prognosis and Quality of Life Impact
Untreated sexual dysfunction significantly worsens quality of life in men with prostatitis. Conversely, addressing erectile concerns early improves treatment adherence, mental health outcomes, and overall patient satisfaction. Long-term prognosis is favorable when a holistic, individualized treatment plan is applied.
Trusted Medical and Research Sources
- National Institutes of Health (NIH) – Prostatitis Overview
https://www.ncbi.nlm.nih.gov/books/NBK599550/ - European Association of Urology (EAU) Guidelines on Chronic Pelvic Pain and Sexual Dysfunction
https://uroweb.org/guidelines - PubMed Systematic Review on Sexual Dysfunction in CP/CPPS
https://pubmed.ncbi.nlm.nih.gov/
Conclusion
Prostatitis—particularly chronic prostatitis and chronic pelvic pain syndrome—can significantly affect erectile strength through inflammatory, neurogenic, muscular, and psychological mechanisms. While prostatitis is not always a direct cause of erectile dysfunction, the association is strong enough to warrant routine sexual health assessment in affected patients. Optimal outcomes depend on comprehensive evaluation and integrated treatment addressing both pelvic pain and erectile function.
Medical Disclaimer
This article is intended for educational and informational purposes only and does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider regarding any medical condition or therapeutic decision.