Why prolonged sitting has become a silent men’s health risk
In modern life, prolonged sitting is no longer an exception; it has become the default posture for millions of men worldwide. Office work, long-distance driving, remote employment, and extended screen time have significantly reduced daily movement. While the negative effects of a sedentary lifestyle on cardiovascular health, metabolism, and the spine are well known, its impact on prostate health remains underestimated. Emerging clinical observations and epidemiological research suggest that extended sitting may negatively influence prostate function, exacerbate existing conditions, and indirectly increase the risk of chronic pelvic disorders. Understanding this relationship is essential for prevention, early intervention, and long-term urogenital health.
Anatomical and physiological background: why the prostate is sensitive to sitting
The prostate is a walnut-sized gland located deep in the pelvis, anterior to the rectum and inferior to the bladder. It surrounds the proximal urethra and plays a central role in male reproductive function by producing prostatic fluid. Anatomically, the prostate lies in close proximity to pelvic floor muscles, venous plexuses, lymphatic drainage pathways, and autonomic nerves.
When the body remains seated for prolonged periods, especially on rigid or poorly designed chairs, mechanical pressure is applied to the perineum. This area contains delicate neurovascular structures directly connected to the prostate. Over time, sustained pressure may impair venous return, reduce microcirculation, and promote pelvic congestion. Unlike muscles that contract and relax with movement, the prostate relies heavily on healthy blood flow and neural regulation to maintain normal function. Any chronic disruption in this balance can increase vulnerability to inflammation and dysfunction.
Prolonged sitting and impaired pelvic circulation
One of the most significant mechanisms linking prolonged sitting to prostate problems is compromised pelvic blood flow. Sitting for long durations compresses the veins of the pelvic floor, slowing venous return and increasing local venous pressure. This phenomenon, often referred to as pelvic venous congestion, can lead to tissue hypoxia and local inflammation.
Reduced circulation affects oxygen delivery and metabolic waste removal within prostate tissue. Over time, this environment may favor inflammatory processes, contributing to symptoms such as pelvic discomfort, urinary hesitancy, and perineal pain. Men who already have a genetic predisposition or a history of prostatitis may be particularly susceptible to these circulatory disturbances.
Inflammation, oxidative stress, and the prostate
Chronic inflammation is a key factor in many prostate-related conditions, including chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) and benign prostatic hyperplasia (BPH). Prolonged sitting can indirectly promote inflammation through physical compression, reduced movement, and metabolic dysregulation.
Sedentary behavior is associated with increased systemic inflammation and oxidative stress. At the cellular level, oxidative stress can damage prostate epithelial cells, disrupt normal glandular secretion, and activate inflammatory pathways. While sitting alone does not cause prostate disease, it can act as a contributing factor that worsens underlying inflammatory processes, especially when combined with poor posture, obesity, or inadequate physical activity.
Impact on prostate pain and chronic pelvic pain syndrome
Clinical evidence indicates that men suffering from chronic pelvic pain syndrome often report symptom exacerbation after extended periods of sitting. This condition, characterized by pelvic, perineal, testicular, or penile pain, is multifactorial but strongly influenced by pelvic floor muscle dysfunction and nerve sensitization.
Prolonged sitting increases tonic contraction in the pelvic floor muscles, leading to muscle fatigue and trigger point formation. These changes can irritate nerves that innervate the prostate and surrounding tissues. Over time, a vicious cycle may develop where pain leads to muscle guarding, which in turn intensifies discomfort and urinary symptoms.
Does prolonged sitting increase the risk of benign prostatic hyperplasia?
Benign prostatic hyperplasia is a common age-related enlargement of the prostate that affects urinary function. While age and hormonal regulation remain the primary determinants, lifestyle factors play a modulatory role.
Several observational studies suggest that physical inactivity is associated with a higher prevalence of lower urinary tract symptoms related to BPH. Prolonged sitting contributes to weight gain, insulin resistance, and systemic inflammation, all of which may influence hormonal metabolism, particularly the balance between testosterone and dihydrotestosterone. Although prolonged sitting is not a direct cause of BPH, it may accelerate symptom progression in susceptible individuals.
Prolonged sitting, prostate cancer, and current evidence
The relationship between sedentary behavior and prostate cancer has been extensively studied, yet remains complex. Current evidence does not conclusively show that prolonged sitting directly increases prostate cancer incidence. However, several large cohort studies indicate that high sedentary time is associated with increased overall cancer mortality, including prostate cancer-specific mortality.
Potential explanations include hormonal dysregulation, metabolic dysfunction, chronic inflammation, and reduced immune surveillance. Importantly, physical activity appears to exert a protective effect by improving insulin sensitivity, lowering inflammatory markers, and supporting immune function. Thus, minimizing prolonged sitting should be viewed as part of a broader cancer risk reduction strategy rather than a standalone prevention measure.
The hidden role of posture and seating ergonomics
Not all sitting is equal. Poor posture amplifies the negative effects of prolonged sitting on the prostate and pelvic structures. Slouched sitting increases pelvic tilt, raises intra-abdominal pressure, and shifts body weight toward the perineum.
Ergonomically inappropriate seating, such as hard, narrow, or non-adjustable chairs, further concentrates pressure on the pelvic floor. Over time, this mechanical stress may aggravate prostate-related symptoms. Proper seating design, combined with postural awareness, can significantly reduce these adverse effects.
How to protect your prostate: evidence-based strategies
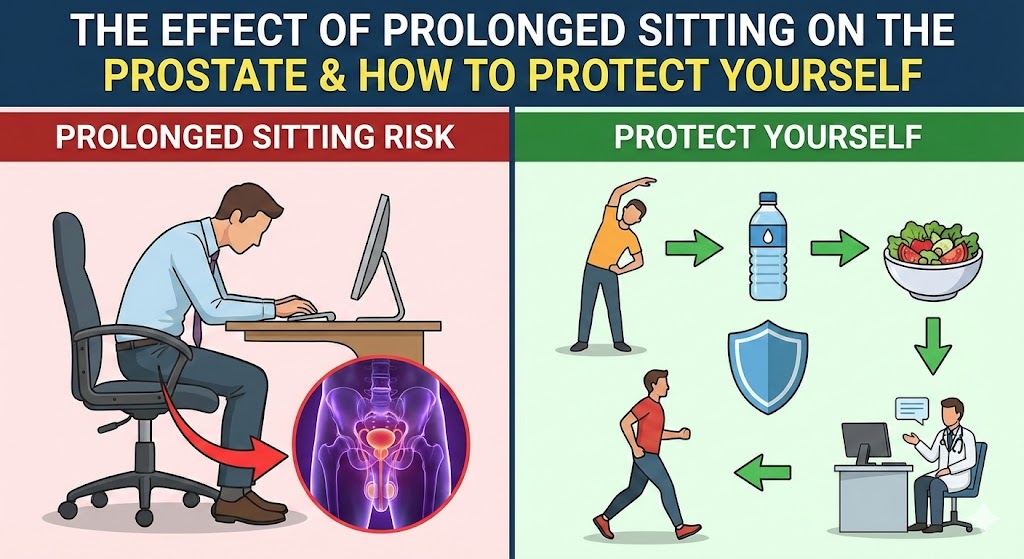
Regular movement breaks
Standing up and moving for even two to five minutes every 30–45 minutes can significantly improve pelvic blood flow and reduce muscle tension. Short walks, gentle stretches, or simply changing posture help restore circulation and prevent pelvic congestion.
Targeted physical activity
Regular aerobic exercise, such as brisk walking or swimming, enhances systemic and pelvic circulation. Strengthening and relaxation exercises for the pelvic floor, when properly guided, support neuromuscular balance and reduce pain associated with prolonged sitting.
Optimizing sitting ergonomics
Using a chair that supports neutral pelvic alignment is essential. The seat should distribute weight evenly across the thighs rather than the perineum. Slight seat tilt, lumbar support, and adjustable height reduce pressure on pelvic structures.
Consideration of sitting aids
Specialized cushions designed to offload perineal pressure may benefit men who must sit for extended periods, such as drivers or desk-based professionals. These aids should promote comfort without destabilizing posture.
Lifestyle modulation
Maintaining a healthy body weight, staying hydrated, reducing chronic stress, and following an anti-inflammatory dietary pattern support overall prostate health. Sedentary behavior rarely acts alone; it interacts with broader lifestyle habits.
Clinical perspective: when to seek medical advice
Men experiencing persistent pelvic discomfort, urinary symptoms, or pain that worsens with sitting should not normalize these signs. Early consultation with a urologist or pelvic health specialist allows for accurate diagnosis, targeted management, and prevention of chronic progression. In many cases, lifestyle modification combined with physical therapy yields significant improvement without invasive interventions.
Authoritative medical and research sources
For readers seeking high-quality scientific information on prostate health and sedentary behavior, the following trusted sources provide evidence-based insights:
– National Institutes of Health (NIH): https://www.nih.gov
– Mayo Clinic – Prostate health and lifestyle factors: https://www.mayoclinic.org
– European Association of Urology (EAU) guidelines: https://uroweb.org
Conclusion: protecting prostate health in a sitting-dominated world
Prolonged sitting is an unavoidable reality for many men, but its impact on prostate health should not be ignored. Through impaired circulation, increased inflammation, and pelvic muscle tension, extended sitting can contribute to discomfort and exacerbate existing prostate conditions. The good news is that practical, evidence-based strategies—regular movement, ergonomic optimization, and lifestyle balance—can markedly reduce these risks. Prostate health is not shaped by a single factor, but by daily habits accumulated over time. Conscious attention to how long and how we sit is a meaningful step toward long-term urogenital wellbeing.
Medical responsibility disclaimer
This article is intended for educational purposes only and does not replace professional medical diagnosis or treatment; any persistent or concerning symptoms should always be evaluated by a qualified healthcare professional.