Prostatitis is one of the most misunderstood conditions in men’s health. Many men try to avoid antibiotics because they want natural solutions, fear side effects, or have taken multiple courses with no improvement. But the reality is this: the answer depends entirely on the type of prostatitis you have.
This article breaks down the complete, science-based truth, showing exactly when prostatitis can be treated without antibiotics — and when antibiotics are absolutely necessary.
Everything here is clear, evidence-based, and easy to understand.
Understanding Prostatitis: The Four Types
Before deciding whether antibiotics are needed, you must know which type of prostatitis you’re dealing with.
1. Acute Bacterial Prostatitis (ABP) – The Emergency Type
This is a sudden and severe infection caused by bacteria.
Symptoms include:
- Fever
- Chills
- Strong pelvic pain
- Burning urination
- Inability to urinate
2. Chronic Bacterial Prostatitis (CBP)
A long-lasting bacterial infection.
Symptoms may come and go:
- Recurrent UTIs
- Painful ejaculation
- Pelvic discomfort
3. Chronic Prostatitis / Chronic Pelvic Pain Syndrome (CPPS)
The most common type.
It is not caused by bacteria.
Main causes include:
- Pelvic floor muscle tension
- Stress
- Inflammation
- Nerve irritation
- Immune dysfunction
4. Asymptomatic Inflammatory Prostatitis
Inflammation found accidentally, with no symptoms at all.
Can Prostatitis Be Treated Without Antibiotics?
Here is the full truth, broken down scientifically.
YES — Prostatitis can be treated without antibiotics IF it is non-bacterial.
This includes:
✓ Chronic Pelvic Pain Syndrome (CPPS)
No bacteria → No need for antibiotics.
This type responds best to:
- Pelvic floor relaxation
- Stretching
- Anti-inflammatory lifestyle
- Supplements
- Stress therapy
✓ Asymptomatic Prostatitis
No symptoms → No treatment required.
Antibiotics have no benefit.
NO — Antibiotics ARE required for bacterial prostatitis.
✓ Acute Bacterial Prostatitis (ABP)
Life-threatening if untreated.
Must be treated with antibiotics immediately.
✓ Chronic Bacterial Prostatitis (CBP)
Requires long-term antibiotics (4–12 weeks).
Without them, infection keeps returning.
Why Antibiotics Don’t Always Work
Many men take antibiotics and see no improvement.
This leads them to believe they “don’t need” antibiotics.
But here’s the truth:
1. Most men don’t have bacterial prostatitis
Over 85–90% of prostatitis cases are non-bacterial (CPPS).
Antibiotics simply cannot fix muscle tension or nerve inflammation.
2. Some bacteria hide inside prostate tissue
Especially in chronic bacterial prostatitis, bacteria can hide in:
- Biofilms
- Deep prostate ducts
This makes them harder to eliminate.
3. Often the problem is pelvic floor dysfunction
Tight pelvic muscles can mimic infection symptoms:
- Burning
- Pain
- Urgency
Antibiotics don’t fix this.
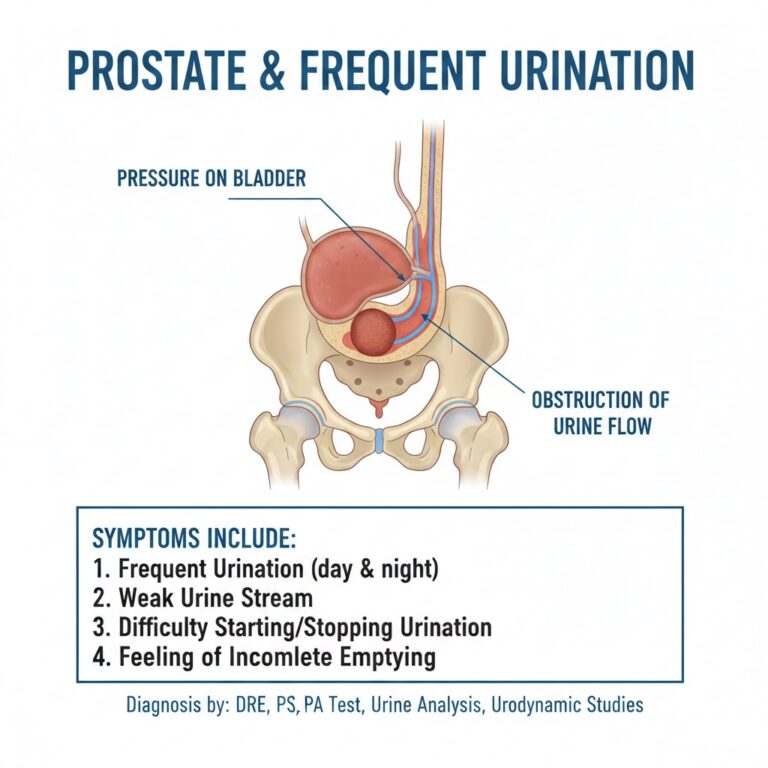
How to Know If You Truly Need Antibiotics
Doctors use specific tests to confirm bacterial infection:
Required Medical Tests
- Urine test (urinalysis)
- Urine culture
- PSA (sometimes elevated)
- Prostate massage test (EPS)
- Semen culture
- Blood tests for severe cases
If bacteria are found → antibiotics are mandatory.
If no bacteria → avoid antibiotics.
Treating Prostatitis WITHOUT Antibiotics (When Safe)
For non-bacterial prostatitis (CPPS), science supports these treatments:
1. Pelvic Floor Physical Therapy
One of the most effective treatments.
It relaxes tight pelvic muscles and reduces nerve irritation.
Benefits:
- Reduces pain
- Improves urination
- Decreases pressure in the perineum
- Helps ejaculation pain
2. Anti-Inflammatory Lifestyle
Foods that reduce inflammation
- Oily fish
- Berries
- Turmeric
- Ginger
- Pumpkin seeds
- Green leafy vegetables
Foods to avoid
- Alcohol
- Caffeine
- Spicy foods
- Processed meat
These reduce swelling in the prostate region.
3. Warm Baths (Sitz Baths)
Relax pelvic muscles and ease pain.
10–15 minutes daily → noticeable improvement.
4. Stress Reduction
Stress tightens pelvic muscles and worsens symptoms.
Recommended:
- Deep breathing
- Meditation
- Counseling
- Stretching
- Yoga
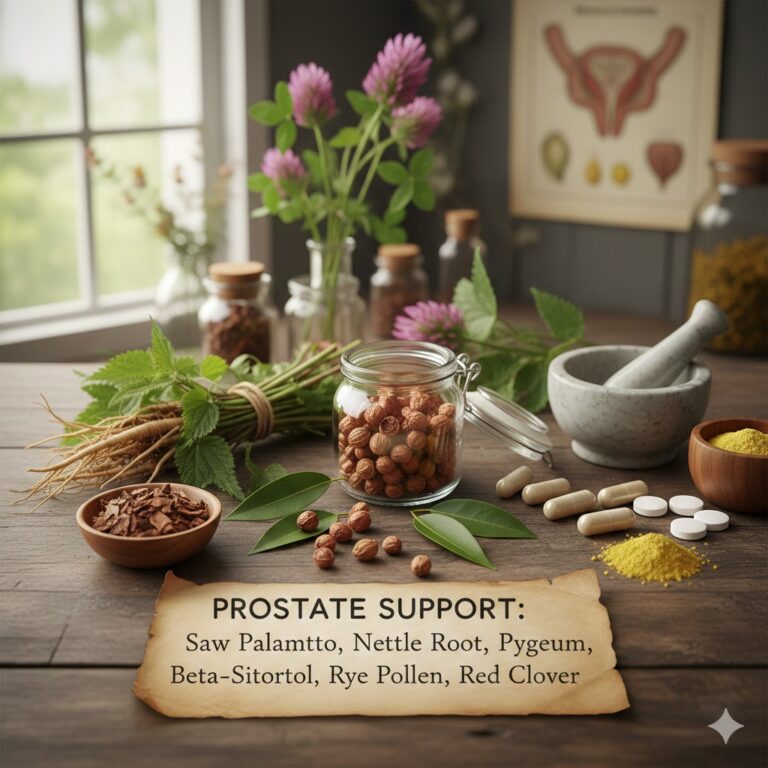
5. Supplements with Scientific Support
✓ Quercetin
Anti-inflammatory flavonoid proven effective in CPPS.
✓ Saw Palmetto
Helps urinary symptoms.
✓ Zinc
Reduces inflammation.
✓ Pollen Extract (Cernilton)
Strong evidence for chronic prostatitis symptom improvement.
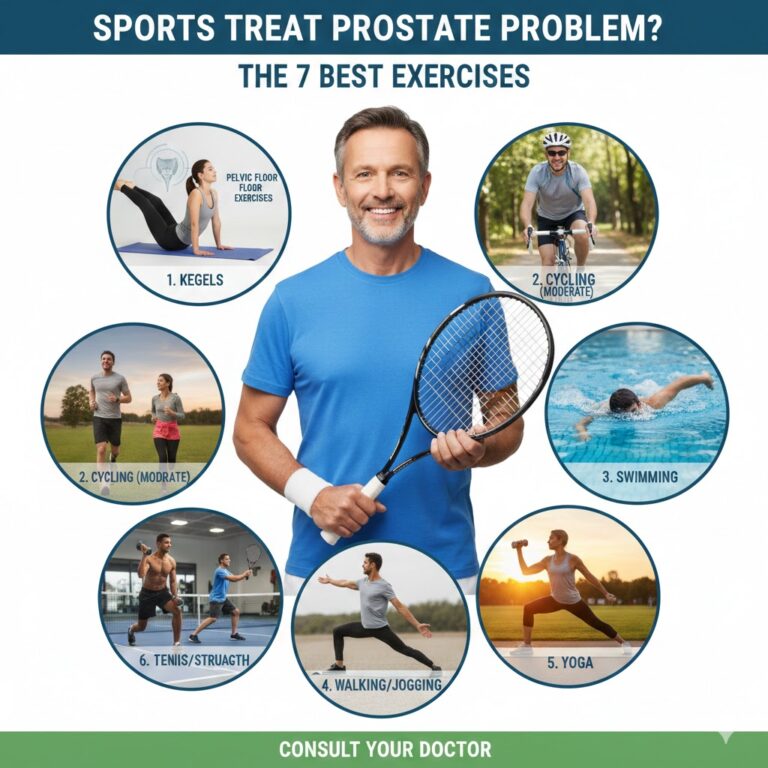
6. Lifestyle Adjustments
Avoid:
- Sitting too long
- Cycling
- Heavy lifting
Do more of:
- Walking
- Stretching
- Light exercise
Treating Bacterial Prostatitis (When Antibiotics Are Required)
If bacteria are confirmed, antibiotics are essential.
Common antibiotics used:
- Ciprofloxacin
- Levofloxacin
- Trimethoprim-sulfamethoxazole
Duration:
- Acute: 2–4 weeks
- Chronic: 6–12 weeks
But even with antibiotics, supportive treatments (listed above) improve recovery.
How Long Does It Take to Recover Without Antibiotics?
If you have non-bacterial CPPS, recovery depends on:
- Muscle tension
- Stress level
- Inflammation
- Lifestyle habits
Typical recovery time:
4–12 weeks with correct treatment.
The Biggest Mistake Men Make
Many men self-treat with antibiotics even when they have no infection.
This leads to:
- Recurring symptoms
- Gut damage
- Antibiotic resistance
- No improvement
The right approach is diagnosis first.
When You MUST See a Doctor Immediately
- Fever
- Chills
- Inability to urinate
- Severe pain
- Blood in urine
- Vomiting
These suggest acute bacterial prostatitis — an emergency.
The Final Truth
You can only treat prostatitis without antibiotics if it is non-bacterial.
- No bacteria = no antibiotics needed
- Bacterial infection = antibiotics required
The key is correct diagnosis, then choosing the right treatment plan.
Trusted Medical Sources (3 High-Authority Links)
1. Mayo Clinic – Prostatitis Overview
https://www.mayoclinic.org/diseases-conditions/prostatitis
2. Cleveland Clinic – Prostatitis Information
https://my.clevelandclinic.org/health/diseases/15313-prostatitis
3. National Institutes of Health (NIH) – Prostatitis Details
https://www.niddk.nih.gov/health-information/urologic-diseases/prostatitis
Final Answer – Can Prostatitis Be Treated Without Antibiotics?
YES — if it is non-bacterial prostatitis (CPPS)
This is the most common type (90–95% cases).
NO — if bacteria are present
Antibiotics are essential for acute or chronic bacterial prostatitis.
Medical responsibility disclaimer
This article is intended for educational purposes only and does not replace professional medical diagnosis or treatment; any persistent or concerning symptoms should always be evaluated by a qualified healthcare professional.

Thanks for this information 🫡